Understanding AV Fistulas

Arteriovenous (AV) fistulas are vital vascular access points for patients undergoing hemodialysis. They are created by surgically connecting an artery to a nearby vein, enabling regulated blood flow for dialysis treatments. This connection allows for the high blood flow rate necessary for effective dialysis while also minimizing complications often associated with other access methods.
The creation of an AV fistula typically involves a straightforward surgical procedure performed by a vascular surgeon. During this operation, the superficial vein is joined to the adjacent artery, a process that induces vascular changes in the area. Over time, the vein dilates and strengthens, becoming suitable for the insertion of dialysis needles. The maturation period for an AV fistula can vary from several weeks to a few months, depending on the individual’s anatomy and overall health. This maturation time is critical, as it ensures the fistula can safely handle the demands of dialysis.
The benefits of AV fistulas compared to alternative vascular access options, such as central venous catheters or AV grafts, are significant. Statistically, AV fistulas demonstrate higher success rates in providing long-term access for hemodialysis, with a failure rate that is significantly lower than other methods. Patients with AV fistulas generally experience fewer complications, such as infections or blood clots, leading to better overall health outcomes. The longevity of av fistulas also contributes to their effectiveness—when properly maintained, these access points can function for many years, promoting a better quality of life for dialysis patients.
In summary, understanding the importance of AV fistulas in dialysis treatment is crucial for patients, caregivers, and healthcare providers alike. They not only serve as a lifeline for those needing regular dialysis but also represent a preferred choice for establishing vascular access in a safe and reliable manner.
The Role of Needles in Dialysis
Dialysis serves as a critical treatment for patients with kidney failure, and the access to the bloodstream is primarily achieved through arteriovenous (AV) fistulas. AV fistula needles play an essential role in this process, allowing healthcare professionals to draw blood for purification and return it once the dialysis has been completed. These needles come in various types that cater to different needs during dialysis sessions. The two main categories of needles are blunt and sharp, each serving a unique function.
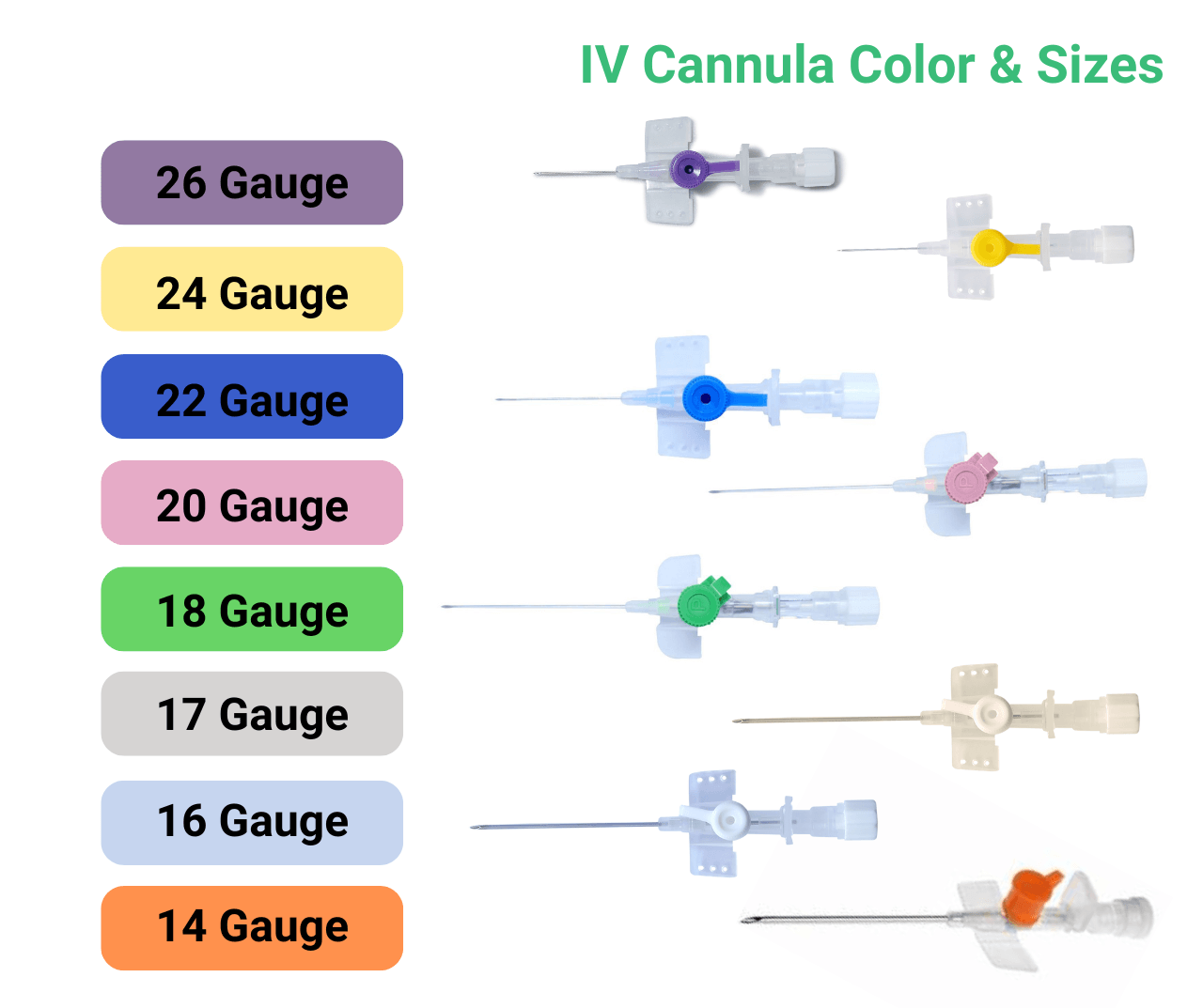
Sharp needles are typically utilized during the initial cannulation of the AV fistula, providing a clean and precise entry point into the vein. Conversely, blunt needles are utilized for the return of blood post-dialysis. The choice of needle size also significantly influences the dialysis process, with standard sizes varying from 15 to 18 gauge. The larger the gauge number, the smaller the needle’s diameter, which can improve patient comfort by reducing the trauma associated with punctures.
The technique used to insert these needles is paramount in ensuring both efficiency and safety. Proper hygiene and technique reduce the risk of complications such as infections and clotting, which can severely hinder the efficacy of the dialysis treatment. Innovations in needle design have emerged to further enhance patient comfort. For instance, newer designs offer a smooth puncture experience and are crafted to minimize pain during insertion, thus improving patient compliance.
As the technology associated with dialysis continues to evolve, advancements in needle design and functionality remain a focal point, providing improved outcomes for patients relying on this life-sustaining treatment. A firm understanding of the role needles play is vital for both healthcare practitioners and patients alike, ensuring that the dialysis process is as pleasant and effective as possible.
Challenges and Complications of AV Fistula Needles
While AV fistula needles serve as a critical component for patients undergoing dialysis, several challenges and complications can arise from their use. One of the most common issues is needle infiltration, which occurs when the needle misses the access site within the fistula. This can lead to discomfort, swelling, and potential tissue damage around the area. Patients must be informed about the signs of infiltration, such as unusual swelling or pain, allowing for timely intervention and adjustment of the needle’s placement.
Another significant concern is clotting within the fistula. Clots can form for various reasons, including low blood flow, inadequate anticoagulation during the dialysis procedure, or even the use of a needle that may not be appropriately sized for the fistula. To address potential clotting, it is crucial for healthcare providers to monitor blood flow rates and assess the patency of the fistula regularly. Patients should also be encouraged to maintain hydration and adhere to prescribed medications that help prevent clot formation.
Infection is yet another critical risk associated with AV fistula needles. These can occur at the site of needle insertion, leading to serious complications if left untreated. Patients should be educated on proper hygiene practices, including handwashing before touching the needle or access site and recognizing early signs of infection such as redness, warmth, or pus around the entry point. Regular communication with healthcare practitioners can facilitate a proactive approach to monitoring both the physical aspects of the fistula and the psychological impacts, such as anxiety related to complications. Awareness and education are paramount in managing these challenges effectively.
Supporting Patients: Tips for Managing AV Fistula Care
Effective management of an arteriovenous (AV) fistula is crucial for dialysis patients to ensure optimal function and longevity of the access point. First and foremost, it is essential for patients to maintain cleanliness at the fistula site. Keeping the area clean reduces the risk of infection, which can lead to complications. Patients should be instructed to gently wash the fistula area with soap and water daily, avoiding any harsh chemicals that might cause irritation.
Moreover, regular monitoring of the fistula for any signs of complications is necessary. Patients should be aware of changes in the area, such as swelling, redness, or unusually cold or pale skin. They should report these symptoms to their healthcare provider promptly. Additionally, it is important to palpate the fistula daily to check for the presence of a “thrill,” which is a buzzing sensation that indicates proper blood flow.
Diet and hydration are also fundamental in managing an AV fistula. Patients should consult with a dietitian who can provide individualized dietary guidelines to promote vascular health. A well-balanced diet rich in fruits, vegetables, and lean proteins can support overall well-being and improve blood flow. Staying adequately hydrated is equally important, as it can help maintain vein health and promote optimal functioning of the fistula.
Lifestyle changes can greatly enhance the effectiveness of an AV fistula as well. Patients should engage in regular, moderate exercise to improve cardiovascular health and circulation. Activities such as walking or gentle stretching can be beneficial. Avoiding heavy lifting or excessive strain on the arm with the fistula is key to preventing injuries or complications.
Lastly, attending regular follow-up appointments is essential in managing care expectations. Patients should understand what to anticipate during their dialysis journey, including necessary adjustments to their care plan. By actively participating in their healthcare management, patients can significantly enhance their overall health outcomes while effectively managing their AV fistula care.